Blood plasma: making all the difference to patients
For the first time in 20 years, we are collecting plasma from UK donors to make life-saving medicines.
Thousands of patients rely on immunoglobulin medicines to treat rare immune diseases. Collection of blood plasma in the UK to make these medicines began in April 2021 for the first time in more than 20 years.
Until this year, the UK depended on blood plasma from other countries. The restriction preventing the use of plasma from UK donors was lifted in February 2021 after it was advised that it is safe.
NHS Blood and Transplant plasma donations will improve the UK’s self-sufficiency in producing its own treatments. Donor centres across England have been taking plasma from several thousand donors. In the first five days of collections starting, 897 donations were made.
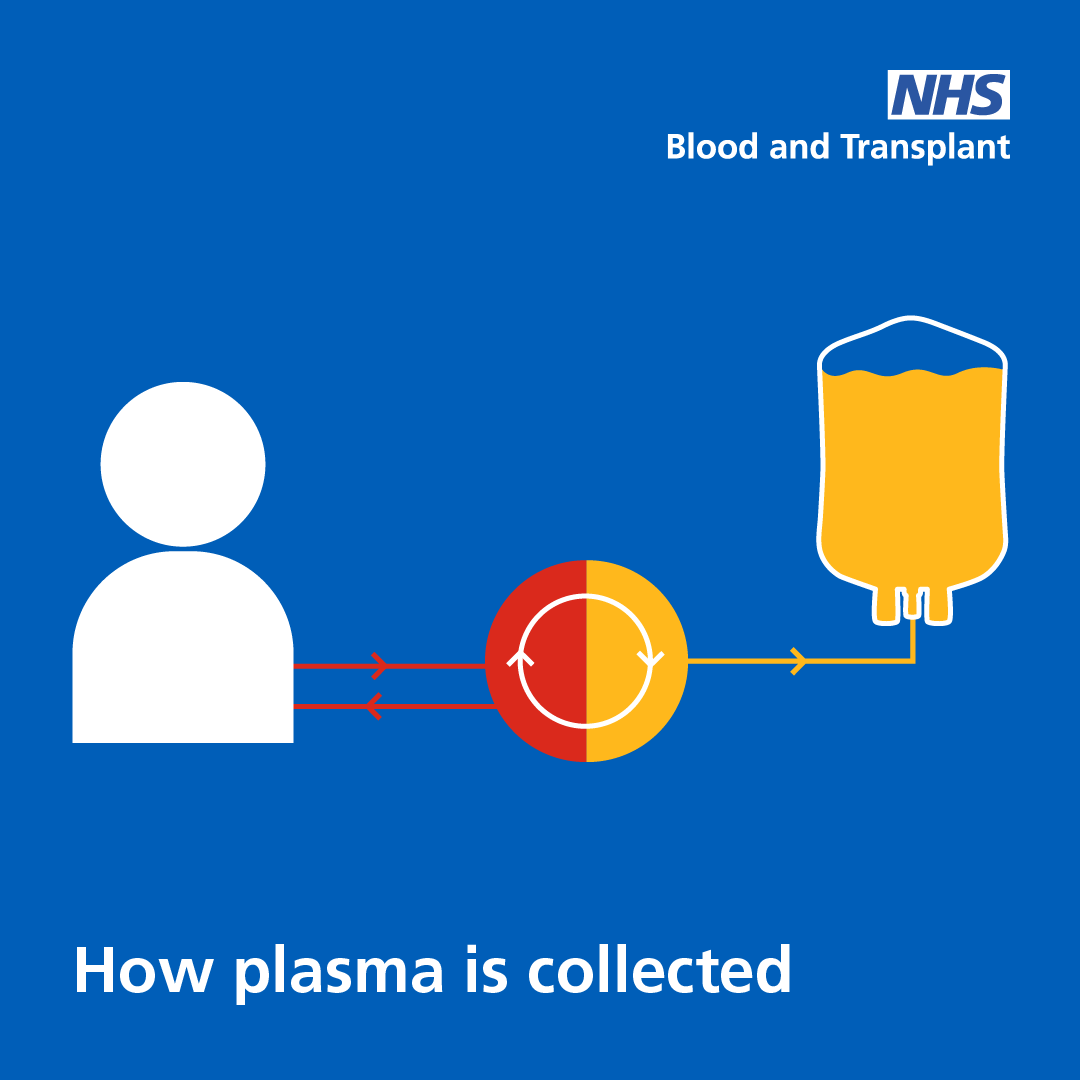
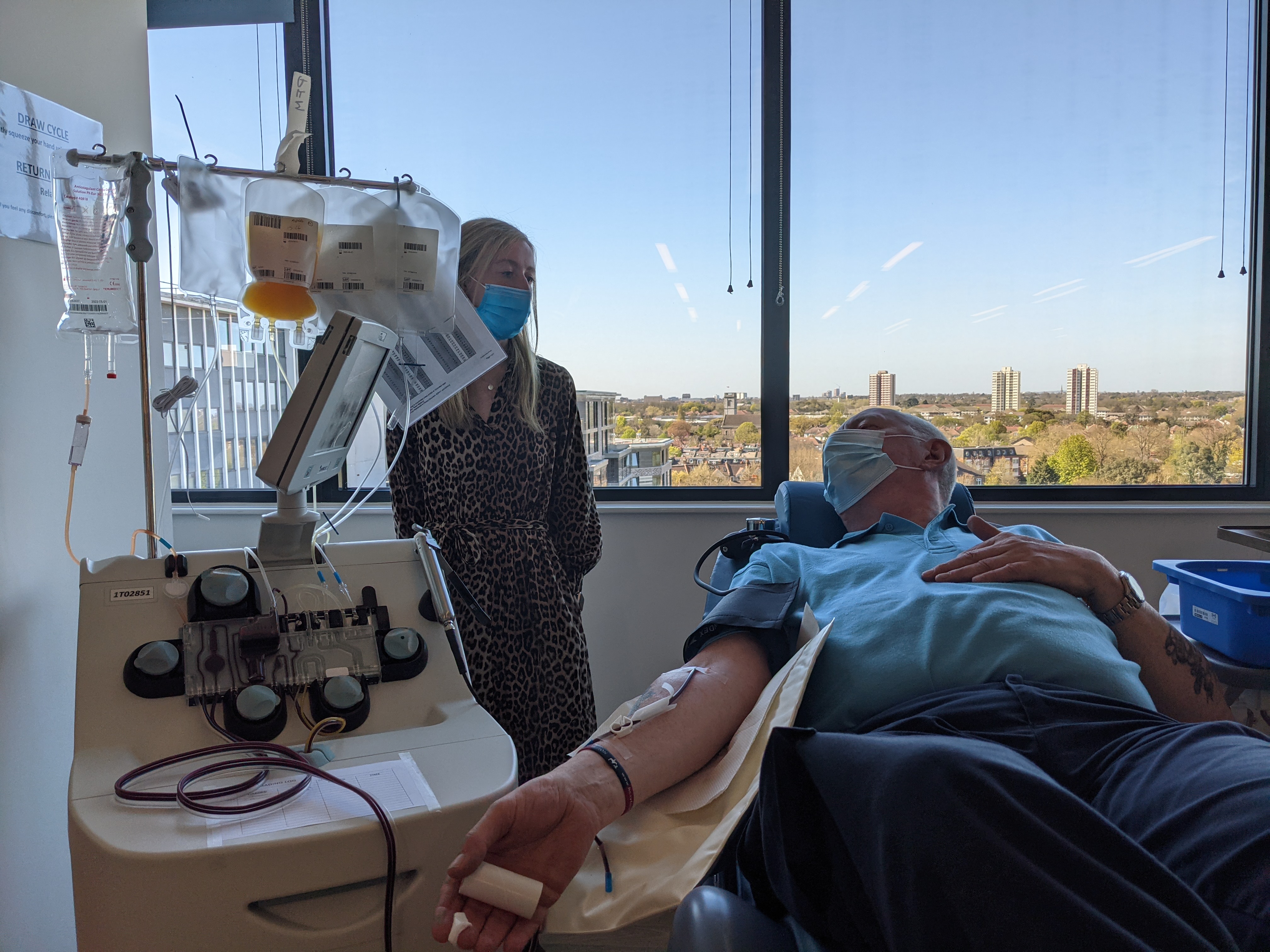
When you give plasma, your blood is processed by an apheresis machine which separates and collects the plasma before returning your red blood cells and other blood components to your body.
The collected plasma is stored and then processed, via fractionation, to separate out the IG immunoglobulins. These are concentrated to make life-saving medicines.
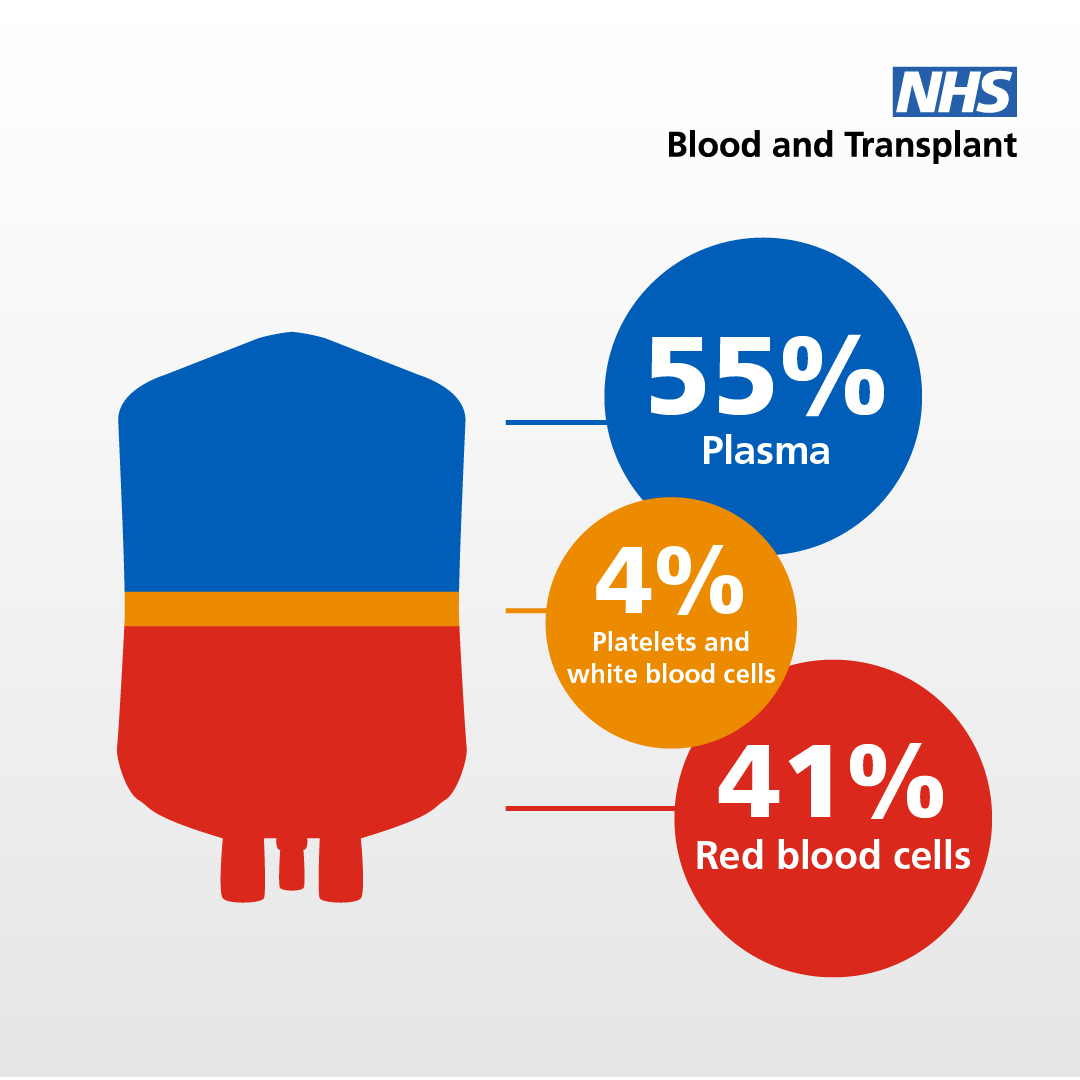
Dr Gail Miflin, chief medical officer for NHS Blood and Transplant, says, “Plasma is made into lifesaving medicines for people with rare diseases. There is a growing need for plasma for medicines and a worldwide shortage of donors. NHSBT already collects some plasma during whole blood donation but a dedicated plasmapheresis programme will greatly increase our ability to provide plasma at volume.
“Like blood donation, plasma donation will be altruistic. We’re asking people we contact to please donate plasma for medicines – you will save and transform lives.”
Who needs immunoglobulins?
Immunoglobulins are used to treat people with weak immune systems and a variety of other rare disorders.
Sue Dimmock, acting chair of UK Primary Immune-deficiency Patient Support, says, “UKPIPS is delighted that UK-donated plasma can now be fully utilised for the benefit of UK patients, to manufacture life-saving immunoglobulin medicines."
Those of us who are unable to make our own antibodies completely rely on regular infusions of donated, plasma-derived antibodies (immunoglobulin) to fight infection and to stay as healthy as possible. Without this treatment, we have an extremely limited defence against infection and disease.
 Erin Sadler, seven, relies on plasma medicines to treat a life-threatening disease, immune thrombocytopenia (ITP). Her immune system destroys her platelets, stopping her blood from clotting. Immunoglobulin medicines help her immune system regulate itself, slowing down the damage.
Erin Sadler, seven, relies on plasma medicines to treat a life-threatening disease, immune thrombocytopenia (ITP). Her immune system destroys her platelets, stopping her blood from clotting. Immunoglobulin medicines help her immune system regulate itself, slowing down the damage.
Erin has a range of other life limiting conditions but lives life to the full, thanks to donors and specialist treatment.
“She is a tornado of energy – cheeky and full of life. She loves dancing and singing. She is vulnerable, but she keeps going,” says Erin’s mum, Helen. “I am so glad there are plasma and blood donors because I would have lost my little girl a long time ago without their selfless act of donation.”
(Picture: Erin relies on plasma medicines)
Erin is very ill with heart failure but still smiling and enjoying herself – she recently asked for nunchucks and practises with them.
Helen says, “We have met many wonderful children who rely on immunoglobulins made from plasma for their survival. I urge anyone who is asked to donate to do so, you will be a life saver!”
 Natalie Beeton, 26, has an immunodeficiency that means she can’t protect herself from infections. She relies on immunoglobulin medicines to protect her from serious illness and help keep her alive.
Natalie Beeton, 26, has an immunodeficiency that means she can’t protect herself from infections. She relies on immunoglobulin medicines to protect her from serious illness and help keep her alive.
Doctors think Natalie’s immune system was badly damaged by a serious case of glandular fever.
“It pretty much killed my immune system,” she says. She was left with a shortage of IgG, the most common antibody, which protects against bacterial and viral infections. Natalie has a transfusion of IgG every six weeks at the Royal Free hospital in London.
(Picture: Natalie receiving an IgG transfusion)
Natalie, an underwriter for a financial company, says, “I was at constant risk of serious infections because my immune system could not stop anything. My illness is long term and I am going to need this medicine for the rest of my life. Donations are the juice that keeps me going.”
 Event manager Charlotte Laycock, 31, needed intravenous immunoglobulin transfusions to help treat a rare long-term condition that causes muscle weakness. She was diagnosed with generalised Myasthenia gravis in January 2021.
Event manager Charlotte Laycock, 31, needed intravenous immunoglobulin transfusions to help treat a rare long-term condition that causes muscle weakness. She was diagnosed with generalised Myasthenia gravis in January 2021.
Charlotte’s immune system attacks the connections between her muscles and her nervous system (CHECK). She suffered muscle weakness, drooping muscles in her eye, lost the ability to speak and most seriously, could not even swallow food for a month.
“I couldn’t eat, I couldn’t talk,” says Charlotte. As you can imagine, my life has been turned a little upside down.”
(Picture: Charlotte receiving immunoglobulin treatment)
She had five days of immunoglobulin treatment at St George’s Hospital in March. She says, “I’m largely symptom free now. I can lead a normal life. It means so much to me that people can now give their plasma. If you can donate, please do – it saves lives.”
Illnesses which are treated with immunoglobulins include immune disorders such as Common Variable Immune Deficiency; neurological disorders such as Guillain–Barre syndrome and Myasthenia gravis; haematological disorders such as Cytopenia - a low mature red blood cell count, which can occur following radiotherapy and chemotherapy for cancer treatment; and dermatological disorders such as Kawasaki syndrome and Toxic epidermal necrolysis.
Dr Matthew Buckland, British Society for Immunology spokesperson and consultant immunologist at Great Ormond Street Hospital and Barts Health NHS Trusts, says, “Plasma products, such as immunoglobulins, are life-saving for patients with conditions that affect the functioning of their immune system. To make these therapies, we rely on the generosity of donors to provide a supply of plasma. There has been a recent increase in global demand for these products, so this new NHSBT programme to enable people in the UK to donate their plasma is hugely welcome.
“It will boost capacity to provide a more sustainable supply of these essential medicines, enabling patients to live their lives without worry about the availability of treatment. Please do consider donating your plasma through the NHSBT programme – your donation will make a world of difference to the patients I treat and allow them to stay well and healthy.”

Donating plasma
Plasma is made into medicines that save and improve the lives of thousands of people with rare diseases.

Other stories
Remarkable stories from the world of giving blood – be they from the research lab, the hospital bed, or the donor chair
