The journey of blood – after you donate
Ever wondered what happens to your blood after you have donated?
Donations will arrive at one of our three manufacturing sites in Manchester, Filton (Bristol) or Colindale (London). We employ around 250 staff who are working different shifts 24 hours a day, 365 days a year, making sure components are available for patients. As NHS Blood and Transplant, we are responsible for blood component production, quality monitoring and storage of the finished blood components.
Each blood component requires a different manufacturing process. Let’s take a closer look at what happens.
What can we make from your blood?
Donations are manufactured into different components, depending on blood group and what hospitals need. These include:
| Component | Function | Key uses | Shelf life |
|---|---|---|---|
| Red blood cells | Contain haemoglobin which distributes oxygen around the body to all tissues and organs; carry waste carbon dioxide back to the lungs where it is expelled | Blood loss/anaemia, trauma, surgery, cancer treatment, blood disorders such as sickle cell disease | 35 days |
| Platelets | Essential in helping blood to clot: they clump together to stop bleeding after an injury | Cancer treatment, surgery | 7 days |
| Plasma | Helps maintain blood pressure and volume and supplies vital proteins for blood clotting | Trauma, bleeding disorders | 36 months |
| Granulocytes (type of white blood cells) | Fight against infection | Patients with life-threatening infections who are not responding to antibiotics | 24 hours |
How do we manufacture these components from your donation?
We receive around 5000 donations a day across the three sites, all of which need to be processed within 27 hours of donation to maintain the quality of the final component.
Whole blood undergoes the following processes:

Leucodepletion
Whole blood donations arrive in batches of packs throughout the day.
These are hung at ambient temperature (22 – 24 °C) and the leucocytes (white blood cells) are removed by a filter.
This is mandatory practice in the U.K as white blood cells (except the granulocytes in some cases) in donated blood usually have no benefit to the recipient but can carry pathogens and cause adverse reactions.

Separation
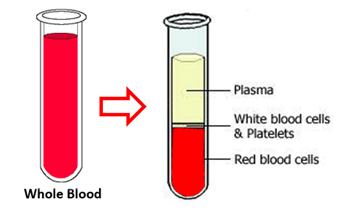
The leuco-depleted units are then centrifuged to separate whole blood into its remaining components.
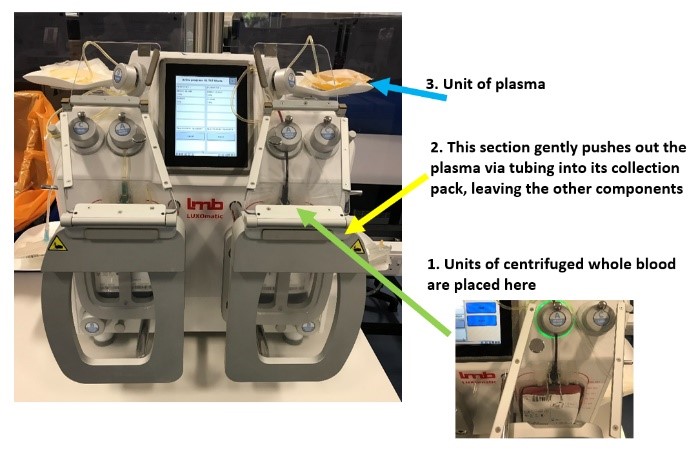 Automated Press
Automated Press
Each unit is then placed in a piece of equipment called a press, which simply pushes the separated components through connected tubing into the appropriate bag within the blood pack system.
The flow of the components to the correct bag is controlled by both weight and light sensors.
Further Manufacturing Steps
Red cells are re-suspended in an additive solution and placed in the fridge. This extends the shelf life, keeps the red cells in optimal conditions and provides the greatest therapeutic benefit to the recipient.
Platelets undergo further processing to pool four donations together with an additive solution to form one adult therapeutic dose.
Plasma is frozen within two hours of separation, which keeps the clotting factors at their highest quality to improve patient outcomes.
Why we separate whole blood into individual components?
It:
- is the most effective way to use each blood donation, as one donation can treat three or more patients
- allows specific treatment by providing a concentrated form of what the patient needs
- meets the clinical demand from hospitals
- allows individual components to be stored in their optimal conditions
What future changes do we see?
There are plans to develop universal plasma. This would mean plasma could be given to any patient regardless of their blood group. This is very exciting, as it would reduce the risk of the patient receiving an incompatible unit, be easier for hospital laboratories to manage their stock and could reduce the demand on the supply chain for specific blood groups.
The human body is so complex and ingenious that artificial blood cannot (yet) replace donated blood. Although work is ongoing in this area, we will need to continue using your donations for many years to come.
Testing, testing, testing!
 When you give blood, we take a little extra for testing later on. It goes into sample tubes which are then tested at our laboratories around the country.
When you give blood, we take a little extra for testing later on. It goes into sample tubes which are then tested at our laboratories around the country.
Find out more about what happens at our testing laboratories.

