Urgent NHS plea for more donors of Black heritage during Sickle Cell Awareness Month
A husband and wife who rely on 200 (1) people a year to save their lives are backing an urgent call from the NHS for more blood donors from the Black community to help people with sickle cell.
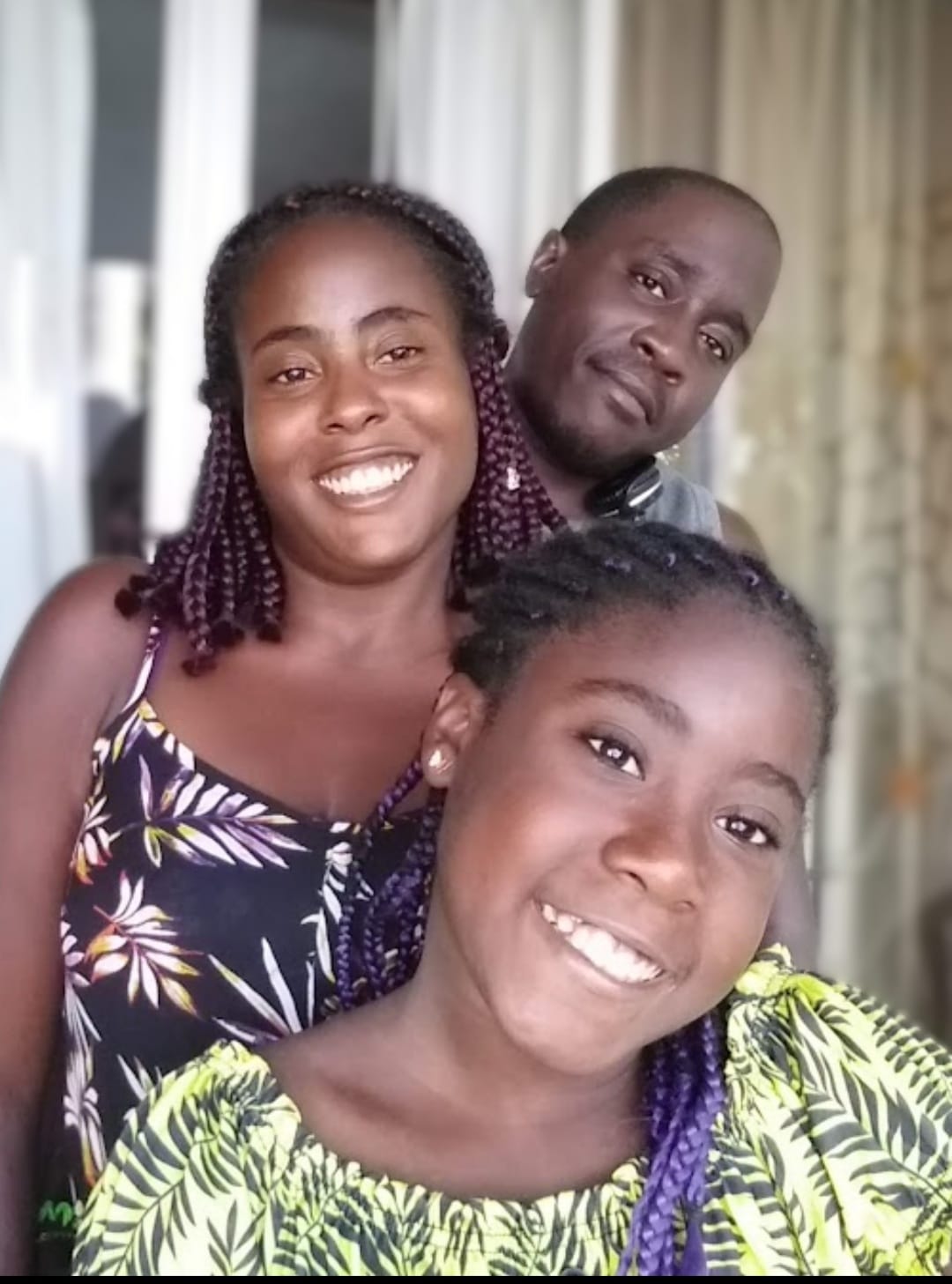 Rebecca Solomon-Henry and Karl Henry from Birmingham (pictured, with daughter Janayah) both have sickle cell and have all their blood replaced by donor blood once a month, a procedure known as a red cell exchange.
Rebecca Solomon-Henry and Karl Henry from Birmingham (pictured, with daughter Janayah) both have sickle cell and have all their blood replaced by donor blood once a month, a procedure known as a red cell exchange.
Sickle cell patients on the exchange programme need donations from 100 (1) people a year on average, according to new statistics from NHS Blood and Transplant.
But only around 50 (2) of these donors are likely to be the best match, putting these patients at risk of serious complications.
New figures also reveal that demand for blood to treat sickle cell patients has gone up by more than 50 percent since 2016 (3). This rise is driven by the greater use of red cell exchanges.
The figures have been released during September’s Sickle Cell Awareness Month to show how blood donation saves and improves the lives of people living with sickle cell. It marks the latest stage in NHS Blood and Transplant’s Giving Type campaign which encourages ‘Giving Types’ to consider becoming a blood donor, particularly those of Black heritage.
Sickle cell is the UK’s fastest growing genetic disorder. It is more common in people of Black heritage and ethnically matched blood provides the best treatment.
But the shortage of Black heritage donors means sickle cell patients do not always get the best matched blood. Where matched blood isn’t available patients are treated with the universal O negative blood type. This is clinically safe but can cause them to develop antibodies which puts them at risk of potentially life-threatening reactions. It also makes it even harder in the long term to find blood they can receive.
I need to continue this treatment to enjoy a longer lifetime with my family
Mum of one Rebecca, 39, has developed antibodies after three years on the exchange programme. She and husband Karl are treated at the NHS Blood and Transplant Therapeutic Apheresis Services unit at Birmingham’s City Hospital. The couple’s 13-year-old daughter Janayah also has sickle cell and has required blood transfusions to cope with serious complications.
Rebecca said: "My blood is becoming harder to match and this makes me wary of having my much needed exchanges every month. I worry my antibodies will continue to build and what this could mean for me in the future.
"The exchanges have been life-changing. My overnight hospital admissions have decreased greatly and I can live life to the fullest.
"In the week before my exchange I’m like a car that’s not functioning well because it’s low on fuel. I become run down, sluggish and in more pain. The donated blood - the fuel - makes everything better.
"I need to continue this treatment to enjoy a longer lifetime with my family. I urge more people of my colour to donate blood. We need you to give all the amazing sickle cell warriors like my husband and my daughter the best chance of an amazing quality of life."
Both Rebecca and Karl, 40, were diagnosed with sickle cell at birth.
Thanks to blood donors, I can watch our daughter grow up and look forward to the future
Karl said: "We had a big celebration for my 40th birthday, as when I was growing up I was told I wouldn’t live to see it. We’ve lost so many friends with sickle cell before they reached 40.
"Sickle cell has ruled my life. I spent most of my childhood in hospital with crisis after crisis. I suffered strokes and lost the ability to walk or talk. I lost my speech for over a year at the age of nine.
"When people ask me how this affected me at school, the answer is simple. I didn’t go to school that much. I wasn’t well enough.
"I’d describe a crisis as feeling like those razor wires you find at the top of fences, pressing into you hard all over your body over and over.
"Blood exchanges help me to feel better and to live better. Thanks to blood donors, I can watch our daughter grow up and look forward to the future."
Sickle cell causes red blood cells to form into sickle or crescent shapes and become stuck in blood vessels, causing episodes of severe pain known as crises, as well as serious or even fatal complications including organ damage and strokes. Donated blood is used in routine and emergency treatment.
Statements
How you can help
Become a blood donor and book your first appointment via the GiveBloodNHS app or our website. If you can’t find an appointment straight away please book for further in the future. Your blood will still help to save lives then.
Press release notes
- Automated red cell apheresis transfusions require between 8 and 10 units of red cells on average per apheresis. Most patients will have an apheresis exchange transfusion every 4 to 8 weeks and on average will need around 100 red cell units every year. In most cases this will be from 100 different donors.
- For Ro units specifically required for sickle cell disorder patients during 2022/23, only 51.3% were fulfilled with O positive and over 48% were substituted with O negative. Similarly, more than half of B positive Ro requests for sickle cell patients were instead substituted with B negative units.
- Total units requested for sickle cell patients was 55,652 in 2015/16 compared with 84,489 in 2021/22.
